|
Cord Blood Used to Treat Child with Hurler Syndrome, Genetic Disorder Meet Lyla Edgington. Lyla was first diagnosed with Hurler Syndrome (MPS Type I) on April 4th, 2016 when she was just 7 months old. Her doctors said she needed a stem cell transplant and that cord blood would give her the best chances at overcoming this life-threatening genetic disorder. Lyla’s doctors and parents began to worry when their pediatrician, Dr. Katherine Lichtsinn at Scottsdale Children’s Group noticed a heart murmur during her 4 month check-up. Returning for another check-up at 6 months, Helen, Lyla’s mother, pointed out a sharp curve in Lyla’s spine that she had noticed. It was then that her doctor suspected a possible genetic disorder and referred them to a specialist at Phoenix Children’s Hospital. In Phoenix, Lyla underwent numerous blood tests hoping to rule out MPS. Unfortunately, this would not be the case. Not only were their fears confirmed but the medical team concluded that Lyla had the most severe form of the disease, MPS Type 1, better known as Hurler Syndrome or Hurler’s disease. "Our world came crashing down that day, but luckily the weeks to follow were full of good news. To say life was like a storm on April 4th, 2016 on the day we received Lyla’s diagnosis, is an understatement…..the tears flowed like a monsoon, my body shook like an earthquake, and the life I envisioned for my daughter was torn to the ground. I truly thought our world had ended." -Helen Edgington, Lyla's Mother Helen was devastated, and worse, she felt responsible even though there was nothing she could have done differently. She and her husband, Steve, had given birth to a beautiful little girl. She was perfect in every way. Hundreds of questions came pouring through the emotions as they wondered “Why us?” MPS I (Hurler, Hurler-Scheie, Scheie syndrome) MPS I, along with six other MPS diseases is a mucopolysaccharide disease that is relentlessly progressive and potentially fatal. MPS I has also been called Hurler, Hurler-Scheie and Scheie syndrome . Hurler takes its name from Gertrude Hurler, the doctor who described a boy and girl with the condition in 1919. In 1962, Dr. Scheie, a consultant ophthalmologist, wrote about some of his patients who were more mildly affected. Individuals who seem not to fit clearly in either the severe or the mild end of the disease were said to have Hurler/Scheie. The specific disease names have been replaced with the designations attenuated (diminished severity) and severe MPS I. There is no cure for MPS diseases, but there are ways of managing and treating the problems they cause. (Source: National MPS Society, http://mpssociety.org/mps/mps-i/ )
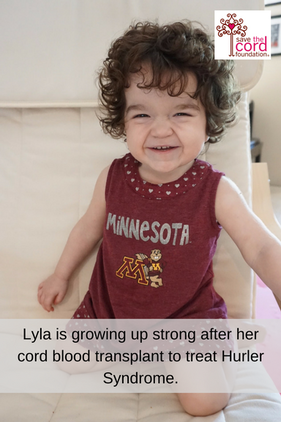
Helen and Steve were encouraged by this possible treatment and agreed that this was their best option for young Lyla. The wheels were put in motion. They would go to Minnesota for treatment. Lyla’s parents received approval from insurance and doctors began to search for a donor. It was a race against the clock as the disease was constantly working against them, deteriorating brain cells. Luckily, a match was found and it was a perfect 6 out of 6 match! The transplant date was set for July 25th, 2016. The procedure lasted 25 minutes and was much like a typical blood transfusion. In accordance with donor rules, Lyla’s parents were not told where the donor was born or the identity of the generous family. They only know that the donated cord blood came from a little girl born in May 2013. She could be from anywhere in the world. "Looking back the reality of the situation, it should have been much scarier than it was. But, we were just so happy and thankful Lyla had the option of a stem cell transplant and that she had a perfect 6 out of 6 cord blood match. We knew there was a long road ahead, but we were very optimistic!" -Helen Edgington, Lyla's Mother 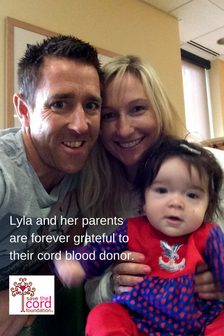 Hurler Syndrome is a progressive genetic disease. If you don’t treat it, it will gradually cause severe physical and mental damage. Lyla’s parents knew this and this is why timing was so crucial in her case. Luckily, Lyla was diagnosed early and did not have too much damage prior to the transplant. This meant her chances were good. However, because of the nature of the disorder, Lyla’s parents and doctors were not expecting to see major improvements necessarily in her mental and physical functions but what they hoped was that the progression of the disorder would stop. The goal was to stop the disorder from becoming worse. Questions remained as to if some damage would continue to occur following transplant or would the transplant be effective immediately? The first few weeks after the transplant were really difficult because of the impact of the chemotherapy. Lyla suffered from low energy and clearly her spirits were down. However, after the first month, doctors confirmed that the transplant had fully engrafted (the donor cells had been accepted by her body). Success! From there it is was smooth sailing. . . she returned to being a happy girl most of the time while living under constant medical supervision (remember, she was not even a year old at the time). When discussing stem cell transplants, doctors often refer to the “first 100 days.” Although not always applicable to every case, this milestone often indicates whether a transplant has been “successful” or not. In Lyla’s case, she was doing great and around day +95 her parents started preparing for their flight home. Then, the phone rang. Lyla’s blood tests came back with issues. Lyla’s parents explained, “The transplant worked but for some unknown reason the new white cells were creating antibodies against the new platelets and red blood cells. Lyla’s immune system needed to be wiped out again to kill the antibodies and we had to hope the new ones wouldn’t do the same thing. This was a huge bump in the road for us and really tore down our spirits. It took another very long 5 months of Lyla on high dose steriods, tons of infusions, very little sleep, and at a huge risk for infection but luckily it worked and the bad antibodies didn’t return! Overall, it took a full 9 months after transplant to know that it was an overwhelming success.”
Advice from Lyla's Parents Looking to the future, we asked Lyla's parents what advice they have for parents, health professionals and even students interested in pursuing STEM careers with an interest in cord blood. For Parents: My advice for parents is to never ignore anything that seems odd about your baby. It took me a month or so to mention the curve in Lyla’s spine because I thought it could have been a normal baby thing or something she would grow out of. For Health Professionals: My advice for health professionals, is to continue to do the amazing work you’re doing and saving so many lives! I have so much appreciation for the medical field and doctors who devote their life to finding cures to all the horrible diseases out there. It’s truly incredible!! For STEM Students:
For students, I encourage you to use your social media skills and networks to help raise awareness for cord blood donation and it’s amazing benefits! In honor of Lyla’s donor and to help build awareness for MPS / Hurler Syndrome as well as the need for cord blood donors, Helen and Steve have created a beautiful video detailing Lyla’s story. Watch the video here. |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
June 2024
Categories |



 RSS Feed
RSS Feed


